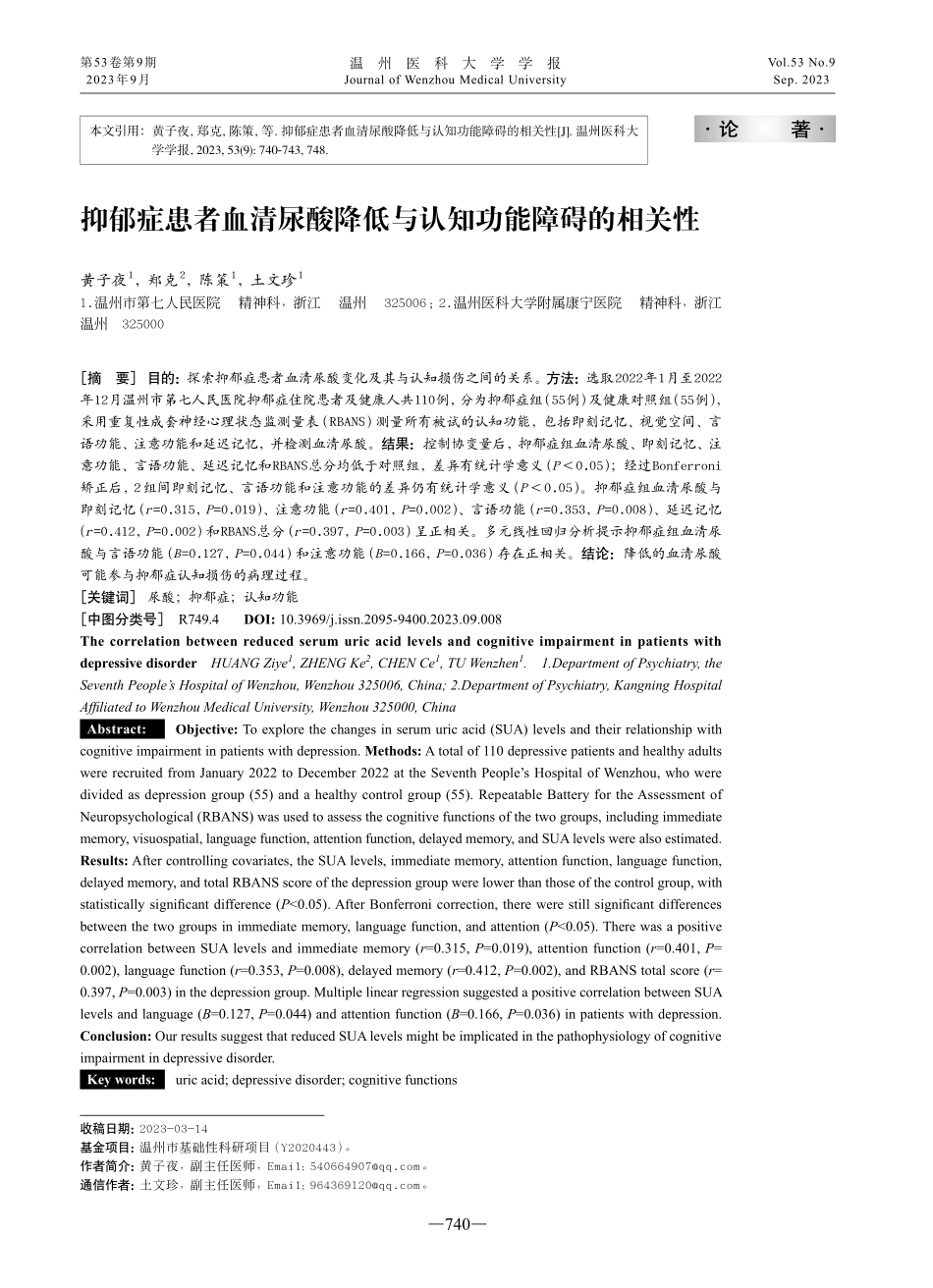
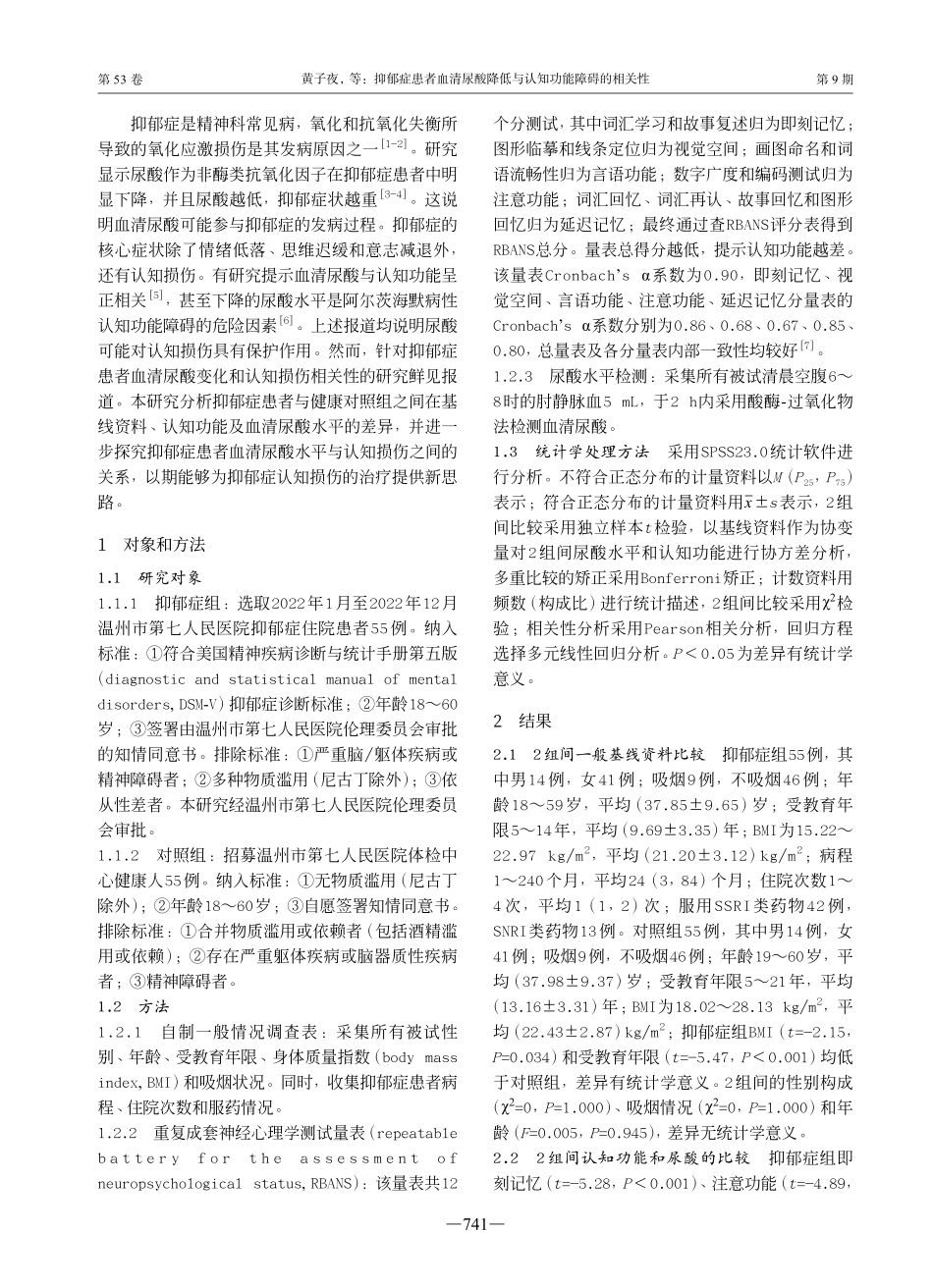
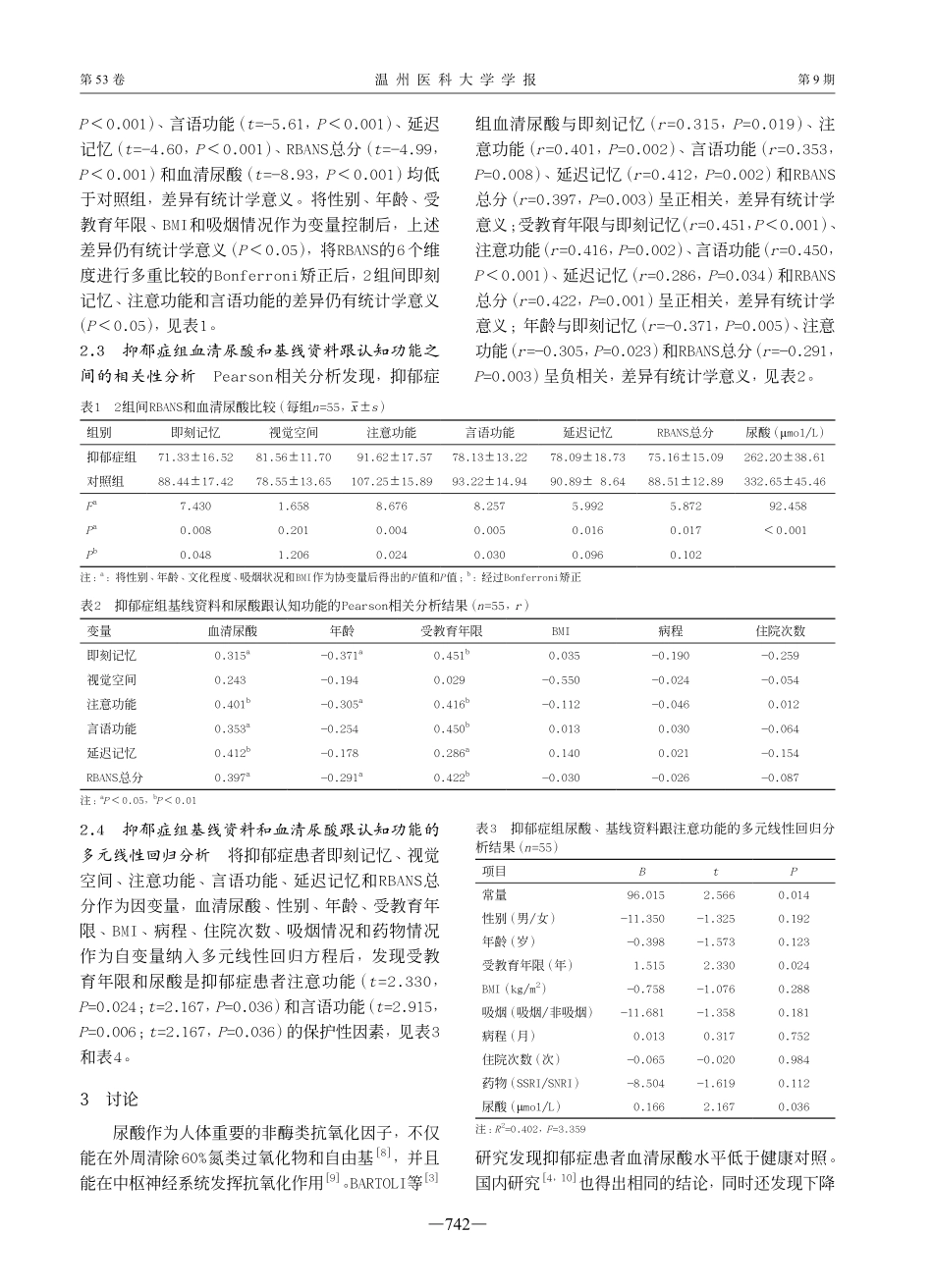
—740—第53卷温州医科大学学报第9期2023-03-14温州市基础性科研项目(Y2020443)。黄子夜,副主任医师,Email:540664907@qq.com。土文珍,副主任医师,Email:964369120@qq.com。收稿日期:基金项目:作者简介:通信作者:抑郁症患者血清尿酸降低与认知功能障碍的相关性黄子夜1,郑克2,陈策1,土文珍11.温州市第七人民医院精神科,浙江温州325006;2.温州医科大学附属康宁医院精神科,浙江温州325000[摘要]目的:探索抑郁症患者血清尿酸变化及其与认知损伤之间的关系。方法:选取2022年1月至2022年12月温州市第七人民医院抑郁症住院患者及健康人共110例,分为抑郁症组(55例)及健康对照组(55例),采用重复性成套神经心理状态监测量表(RBANS)测量所有被试的认知功能,包括即刻记忆、视觉空间、言语功能、注意功能和延迟记忆,并检测血清尿酸。结果:控制协变量后,抑郁症组血清尿酸、即刻记忆、注意功能、言语功能、延迟记忆和RBANS总分均低于对照组,差异有统计学意义(P<0.05);经过Bonferroni矫正后,2组间即刻记忆、言语功能和注意功能的差异仍有统计学意义(P<0.05)。抑郁症组血清尿酸与即刻记忆(r=0.315,P=0.019)、注意功能(r=0.401,P=0.002)、言语功能(r=0.353,P=0.008)、延迟记忆(r=0.412,P=0.002)和RBANS总分(r=0.397,P=0.003)呈正相关。多元线性回归分析提示抑郁症组血清尿酸与言语功能(B=0.127,P=0.044)和注意功能(B=0.166,P=0.036)存在正相关。结论:降低的血清尿酸可能参与抑郁症认知损伤的病理过程。[关键词]尿酸;抑郁症;认知功能[中图分类号]R749.4DOI:10.3969/j.issn.2095-9400.2023.09.008ThecorrelationbetweenreducedserumuricacidlevelsandcognitiveimpairmentinpatientswithdepressivedisorderHUANGZiye1,ZHENGKe2,CHENCe1,TUWenzhen1.1.DepartmentofPsychiatry,theSeventhPeople’sHospitalofWenzhou,Wenzhou325006,China;2.DepartmentofPsychiatry,KangningHospitalAffiliatedtoWenzhouMedicalUniversity,Wenzhou325000,ChinaAbstract:Objective:Toexplorethechangesinserumuricacid(SUA)levelsandtheirrelationshipwithcognitiveimpairmentinpatientswithdepression.Methods:Atotalof110depressivepatientsandhealthyadultswererecruitedfromJanuary2022toDecember2022attheSeventhPeople’sHospitalofWenzhou,whoweredividedasdepressiongroup(55)andahealthycontrolgroup(55).Repeata...